COVID-19: What to Do If You Are Sick
- Category: Did You Know?
- Posted On:
So – you have been diagnosed with COVID-19. Now what?
Receiving treatment in a timely manner is especially important for unvaccinated individuals, who are 17 times more likely to be hospitalized and 11 times more likely to die of the virus than vaccinated individuals.
Signs & Symptoms to Watch For
According to the CDC, people with COVID-19 have had a wide range of symptoms reported – ranging from mild symptoms to severe illness. Symptoms may appear 2-14 days after exposure to the virus. Anyone can have mild to severe symptoms.
People with these symptoms may have COVID-19:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Warning Signs of Worsening Illness
- Trouble breathing
- Persistent pain or pressure in the chest
- New confusion
- Inability to wake or stay awake
- Pale, gray, or blue-colored skin, lips, or nail beds, depending on skin tone
Monitor Your Health from Home
The best place to recover if you have a mild case of COVID-19 is at home, where you can eliminate the spread of the virus to others. Avoid physical contact with family members and maintain a distance of six feet. Any household member who had close contact with you before you tested positive should quarantine (stay home) until you are able to get specific instructions for them from your provider. To keep your strength, make sure to hydrate, rest, and eat, even if you aren’t hungry.
Watch Your Temperature
Track your symptoms while at home. One of the best ways to do this is with a thermometer. A temperature of 100.4 degrees or higher can be a sign that you have a fever caused by a worsening illness or infection.
Track Your Pulse
Because COVID-19 can cause an irregular or high heart rate (over 100 beats per minute), you should keep track by regularly measuring your pulse. Count the number of beats you feel in your wrist or neck for 60 seconds, or count the beats for 30 seconds and multiply it by two. Normal resting heart rate is between 60 and 100 beats per minute and can be slower if you exercise a lot or take medications like beta-blockers.
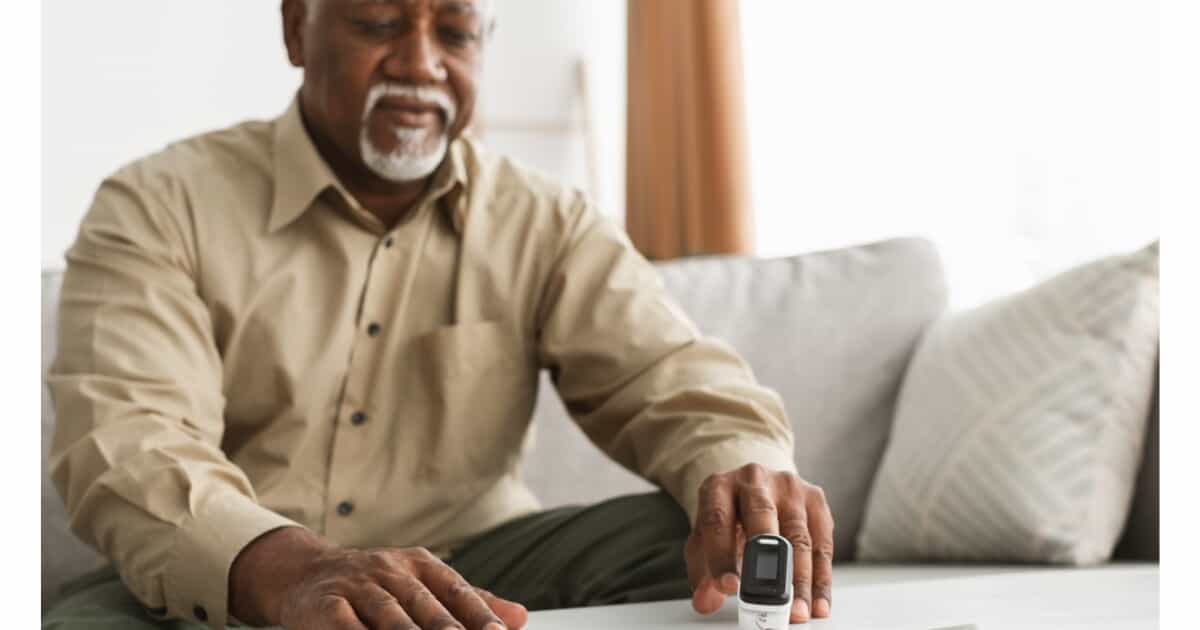
Try a Pulse Oximeter
This tool isn’t one you find in every medicine cabinet, but it can be helpful in detecting worsening oxygen levels. Placed on a fingertip, a pulse oximeter uses light beams to estimate the amount of oxygen carried in the blood (oxygen saturation) and pulse rate.
Patients with conditions such as COVID-19 who monitor their condition at home should pay attention to all worsening symptoms and communicate any concerns to their healthcare provider. A normal pulse oximetry reading is typically 95% or higher. Some individuals with chronic lung conditions may have readings around 90%. If your home pulse oximeter readings consistently trend lower than 90%, contact your healthcare provider.
Please note - The FDA has informed users that pulse oximeters have limitations. Pulse oximeters cannot be used to diagnose or rule out COVID-19.
When Monoclonal Antibody Treatment is Appropriate
Some patients with mild to moderate COVID-19 may benefit from the infusion of COVID-19 monoclonal antibodies to prevent progression to severe disease resulting in hospitalization or death. This therapy is not a replacement for vaccination, which is the best way to prevent hospitalization and death from COVID-19. If you or your child 12 or older have tested positive for COVID, contact your provider’s office to see if you or your child are in the higher risk group that should have an antibody infusion. If you are, your provider will offer to schedule you. Click here to learn more about monoclonal antibody treatment at Valley Health.
When to Seek Emergency Care
If your symptoms are getting worse and/or you have the warning signs above*, do not delay – get help right away. A doctor’s office or Urgent Care is not the appropriate place to seek help in an emergency. If you feel you need emergency care, share your concerns with the 911 dispatcher and Emergency Medical Services (EMS). EMS personnel can begin life-saving treatment immediately, even before you get to the hospital. If you choose to drive to an Emergency Department, you should stay in your car and call the number that is posted at each entrance. For additional information about coronavirus symptoms and when to seek medical attention, please visit the CDC website.
Prevention: The Importance of Vaccination
According to the Virginia Department of Health, of Virginians who are fully vaccinated against COVID-19, less than 1% have developed COVID-19. Even fewer have had to be hospitalized or have died. This is why it’s so important to get vaccinated as soon as possible.
If you are unvaccinated and recovering from COVID-19, talk to your doctor about when you can get vaccinated to boost antibody levels. Those who have had mild or severe infections, or have received monoclonal antibodies, may need to wait a few months before getting vaccinated.
Learn more about local vaccination efforts at www.valleyhealthlink.com/vaccine.


